My Webinar on Women Urinary Incontinence.
For those who are suffering from urinary incontinence and need to understand it better, the webinar tries to explain what it is, why it happens and how can it be treated.
As aging occurs, women go through changes in their appearance. Most obviously is in the face.
So WHAT is URINARY INCONTINENCE?
Urinary incontinence is the involuntary leakage of urine. It means a person urinates when they do not want to. Control over the urinary sphincter is either lost or weakened.
WHY does it occur?
Incontinence
of the bladder occurs when those pelvic muscles that involves in urination get traumatized,
either overstretched or tear,
that leads to weakness of the muscles. As
time goes by, the muscles become weaker until at certain point, they cannot
support the bladder anymore. When there is high
pressure from the abdomen such
as coughing, sneezing, lifting or
pushing heavy things,
the bladder forces urine past the urethral sphincter causing incontinence to
occur.
There are several CLINICAL FEATURES to look out for in Urinary Incontinence depending on which type of incontinence one has,

For those who are suffering from urinary incontinence and need to understand it better, the webinar tries to explain what it is, why it happens and how can it be treated.
As aging occurs, women go through changes in their appearance. Most obviously is in the face.
But aside from the face and facial features, our body goes through changes as well in it shape as well as function. From babyhood to girlhood to young lady then a woman and middle age and elderly lady, these changes is affected due to physical changes as well as hormonal changes.
Some changes are obvious like skin laxity, white hair and weight gain, while others are subtle and barely felt or seen until it begins to affect our routine and lifestyle. One of them is urinary incontinence.
Urinary incontinence is the involuntary leakage of urine. It means a person urinates when they do not want to. Control over the urinary sphincter is either lost or weakened.
WHY does it occur?
WHAT are the TYPES of Urinary Incontinence ?
There
are four main types
of Urinary Incontinence (UI):
1.
Stress incontinence due
to poor closure of the bladder (SUI).
2.
Urge Incontinence due inability to hold urine flow
3.Mixed
Incontinence presence of
both condition
4.
Overflow incontinence due
to either poor bladder contraction or blockage of the urethra.
STRESS
URINARY INCONTINENCE occurs when
1) Cough
2)
Sneeze
3)
Laughing
4)
Lifting heavy objects
5)
Vigorous exercise
6)
Have sexual intercourse
7) Standing
in
prolonged time
while
URGE
INCONTINENCE presents with
1)
Frequent urination, in a day and at nighttime
2)
Sudden urination and urinary urgency
and
OVERFLOW
INCONTINENCE features :
1)
Bladder never feels empty.
2)
Inability to void when the urge is felt
3)
Urine dribbles even after voiding
WHAT CAUSES urinary incontincne?
Incontinence
may be a temporary problem caused by a vaginal or urinary tract infection
(UTI), constipation, certain medications, or it can be a chronic condition.
The
most common causes of chronic incontinence include :
Overactive bladder
muscles and Weakened pelvic floor muscle
These are due to Weakening of the urethral sphincter and pelvic floor muscles due to pregnancy, childbirth, aging, obesity, menopause, surgical procedures (eg hysterectomy)
1. Aging
Aging
is natural and just as your skin begins to show signs of this process by
becoming thinner or developing wrinkles, aging is bound to take its toll on
your vagina as well. Once you hit menopause, it all boils down to hormones, in
this case, estrogen.
Estrogen, the
female sex hormone, is involved in the growth, maintenance, and repair of
reproductive tissues. The natural decline in
the body’s estrogen
levels begins during perimenopause, which is the period of transition before
hitting menopause and usually starts in the late 30s.
Low levels of oestrogen cause a number of health issues in women like stroke, heart disease and osteoporosis. Changes to the vagina include lesser secretion of natural lubricants, which in turn lead to dryness and itchiness, thinning of vaginal walls and loss of elasticity, further contributing to vaginal looseness.
Vaginal
atrophy (atrophic vaginitis) is thinning,
drying and
inflammation of the vaginal walls
due to your body having less estrogen. Vaginal
atrophy occurs
most often after menopause. For many women, vaginal
atrophy not
only makes intercourse painful, but
also leads to distressing symptoms.

Vaginal
dryness
Vaginal
burning
Vaginal
discharge
Genital
itching
Burning
with urination
Urgency with
urination
More
urinary tract infections
Urinary
incontinence
Light
bleeding after intercourse
Discomfort
with intercourse
Decreased
vaginal lubrication during sexual activity
Shortening
and tightening of the vaginal canal
2. Childbirth.
In women, poor function of pelvic floor muscles or the sphincter may occur because of tissue or nerve damage during delivery of a child. Stress incontinence from this damage may begin soon after delivery or occur years later.
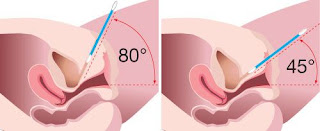
AS you can see from this 2 diagrams the urethra which is the outlet of the bladder for urine to flow out lies just in front of the vagina. Because the 2 structures lie so close together, infact the urethra almost lies on top of the front wall of the vagina, you can see how the laxity and thinning of the vagina wall will affect the urethra.
Other factors that may worsen stress incontinence include:
3.Illnesses that cause chronic coughing or sneezing
4. Obesity
5. Smoking, which can cause frequent coughing
6. High-impact activities, such as running and jumping, over many years
If
you have stress incontinence, you may experience urine leakage when you Cough, Sneeze, Laugh, Stand
up, Get
out of a car, Lift
something heavy, Exercise or even when you have
sex
HOW can we treat or manage SUI?
I devide it into Non Medical, Medical and NonSurgical & Surgical.
Non Medical remedies include :
Own TREATMENT
1. Pelvic floor muscle exercises. This exercise strengthens pelvic floor muscles and is effective for a range of pelvic issues like pelvic prolapse and incontinence. Kegel exercises strengthen the pelvic floor muscles and urinary sphincter.
2. Fluid consumption. The amount and timing of fluids consumed during the day and evening.
3. Healthy lifestyle changes.
4. Bladder training.
Lifestyle Tips
For many people with incontinence, the following self-help tips and lifestyle changes are enough to relieve symptoms.
1. Do daily pelvic floor exercises.
2. Quit smoking.
3. Do the right exercises.
4. Avoid lifting.
5. Fight incontinence by losing weight.
6. Treat constipation promptly.
7. Cut down on caffeine.
MEDICAL Remedies include :
1.Vaginal moisturizer (K-Y Liquibeads, Replens, others) to restore some moisture to your vaginal area. You may have to apply the moisturizer every two to three days. The effects of a moisturizer generally last a little longer than those of a lubricant.
2.Water-based lubricant (Astroglide, K-Y jelly, Sliquid, others) to reduce discomfort during intercourse. Choose products that don't contain glycerin because women who are sensitive to this chemical may experience burning and irritation. Avoid petroleum jelly or other petroleum-based products for lubrication if you're also using condoms. Petroleum can break down latex condoms on contact.
3. Topical (vaginal) estrogen. Vaginal estrogen has the advantage of being effective at lower doses and limiting your overall exposure to estrogen because less reaches your bloodstream. It may also provide better direct relief of symptoms than oral estrogen does.
Medications that are available and may help are :
1. Anticholigernics which are medications that help to "calm" the bladder. This is usrful mainly for Urge Incontinence
2. Antidepressants like Imipramine and Duloxetine
3. Topical oestrogen can be used to help with the laxity of vagina
4. Alpha & Beta adrenergic antagonists like phenylpropanolamine
Medical Devices that can used include
1.Urethral insert (Femsoft insert)
2. Pessary
Lastly Surgery might be offered like
1.SLing procedures
2.Bladder neck suspension
3.Artificial usirnary sphincter
Vaginal Rejuvenation
Non-Surgical
Non-surgical vaginal
rejuvenation can be in the form of laser treatments where
heat is applied to the tissues to stimulate collagen formation, thus resulting
in a taut vagina.
Use
of vaginal fillers and threads is
also common to lift tissues and bring about a tightening effect.
Targeting
the walls of the vagina is possible with the wide variety of vaginal
rejuvenation products like creams, serums, and herbal soaps available in the
market.
Surgical
There are a number of cosmetic procedures such as revirgination or hymenoplasty,
clitoral unhooding, and G-spot amplification that fall under the broad category
of vaginal rejuvenation procedures. When it comes to the tightening of vaginal
walls and muscles, invasive reconstructive surgery proves to be an effective
option.
Surgery
can help shorten or change the shape of the vaginal muscles and tissues.
Enhancing the fullness of vaginal tissue is also made possible through fat
transplantation.
Vaginal Rejuvenation Procedures
Vaginal
rejuvenation is all about improving the health and vitality of the vaginal
walls and muscles and can be done both surgically and non-surgically. Here’s a
look at some procedures and methods.
—Lasers
– Mona Lisa, Incontilase
—Radio
Frequency - Viveve
—Ultrasound
—Others
– Emsella, Fermilift
In my practice , I use Incontilase and Viveve for treating of mild to moderate Stress Urinary Incontinence, Sexual Dysfunction, Atrophic Vagina, Vaginal LAxity as well as 1st degree Uterine Prolapse.
IncontiLase® is
a patent-pending, non-invasive Er:YAG laser therapy
for the treatment of mild and moderate stress
urinary incontinence,
based on non-ablative photothermal
stimulation of collagen neogenesis,
shrinking and tightening of vaginal
mucosa tissue and collagen-rich endopelvic
fascia, and subsequently greater ...
The treatment
is generally painless. Improvement
of the connective tissue and therefore of the firmness of the vagina, makes
that about 85% of the treated women no longer suffer from urinary incontinence.
Patient can immediately return her normal activities after treatment.Apr 23,
2018
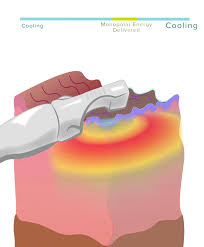
Viveve® is
the Non-surgical radio frequency
treatment to help with urinary incontinence and vaginal
laxity
The Viveve device
delivers a noticeable tightening of the vagina for increased friction and
pleasure during sexual intimacy, greater bladder control, and more youthful
vaginal tissue.
“Geneveve
by Viveve uses cryogen-cooled monopolar
radiofrequency to
uniformly deliver gentle volumetric heating while
cooling surface tissue. This device tightens the vagina; increasing
moisture and improving urinary incontinence in women. It
works largely by stimulating the body's natural collagen formation
process.”
If you do, please seek help. It is never too late and the earlier you treat the better the outcome and the lesser you need. Don't let Bl;adder Leakage hold you back in your activities, travels and carrying out your routines.
You can listen to the whole webinar at this link
https://youtu.be/eBMtjbLYGt0
I can be reached at my FB page DrSutina Nordin , email drsutina@gmail.com or WA 0123282840.




















Comments